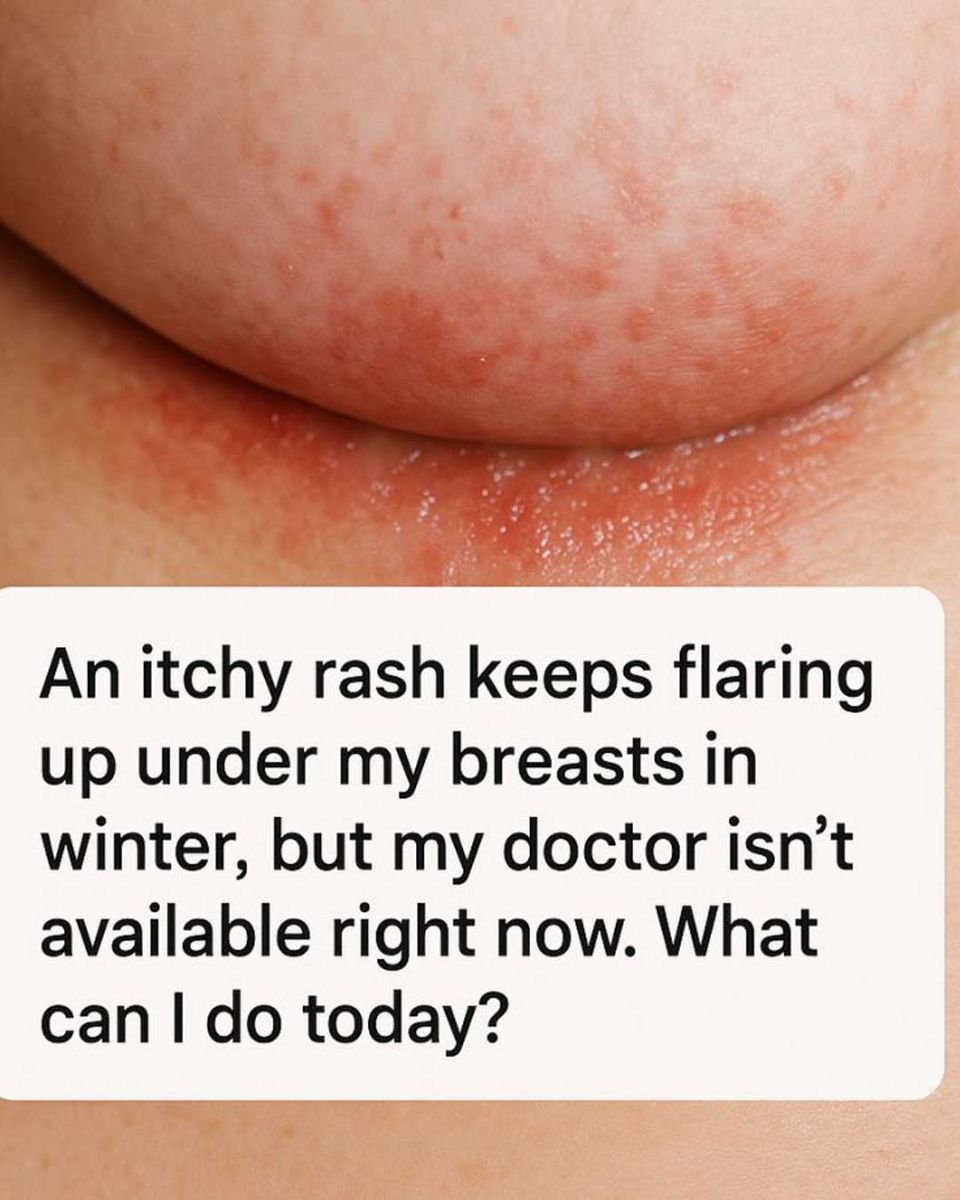
An itchy, irritated rash under the breasts can be incredibly uncomfortable, frustrating, and even embarrassing. You’re not alone—this is a very common problem, especially during the winter months when heavier clothing, indoor heating, and reduced airflow create the perfect conditions for skin irritation.
The good news is that there are practical, safe steps you can take today to calm the rash, reduce itching, and prevent it from getting worse while you wait to see your doctor.
Why This Rash Happens More Often in Winter
The skin under the breasts is a natural skin fold. That area tends to trap moisture, heat, and friction, which weakens the skin barrier over time. In winter, several factors make this worse:
- Heavier bras and layered clothing reduce airflow
- Indoor heating dries the skin, making it more prone to cracking and irritation
- Sweat gets trapped even when you don’t feel “hot”
- Friction increases when skin is dry and sensitive
This combination often leads to intertrigo, a skin-fold rash that can become itchy, red, and sore. Yeast or fungal overgrowth frequently develops on top of the irritation, which intensifies the itching and redness.
Common Symptoms You Might Notice
- Red or pink patches under the breasts
- Itching or burning sensation
- A raw or irritated feeling
- Mild scaling or shiny skin
- Worsening symptoms with sweat or tight clothing
If the rash keeps coming back in winter, that strongly suggests moisture and friction are key triggers.
What You Can Do Today for Relief
1. Clean Gently — Once a Day Is Enough
Wash the area gently with lukewarm water and a fragrance-free, mild soap. Avoid scrubbing. Pat dry carefully instead of rubbing.
After bathing, use a cool hair dryer on the lowest setting for about 30–60 seconds to make sure the area is completely dry. This step alone can significantly reduce irritation.
2. Apply an Over-the-Counter Antifungal Cream
Because yeast is often involved, using an antifungal cream is a safe and effective first step.
Look for:
- Clotrimazole 1%
- Miconazole 2%
- Ketoconazole 1%
Apply a thin layer twice daily to clean, dry skin. Continue for 7–14 days, even if symptoms improve sooner. Stopping too early can cause the rash to return.
Avoid using steroid-only creams unless a healthcare provider specifically advised it. Steroids can temporarily reduce redness but may worsen fungal rashes over time.
3. Protect the Skin With a Light Barrier
Once the antifungal cream has absorbed, you can protect the skin from moisture and friction by applying a very thin layer of:
- Zinc oxide cream
- Petroleum jelly
This helps prevent rubbing and keeps sweat from sitting directly on the skin.
4. Reduce Moisture and Friction Throughout the Day
- Go braless at home when possible
- Choose breathable cotton bras instead of synthetic fabrics
- Place a soft cotton cloth or gauze under the breast to absorb moisture
- Change bras if they become damp
Small adjustments like these can make a big difference.
What to Avoid (These Can Make It Worse)
- Cornstarch or scented powders (they can feed yeast)
- Fragranced lotions or sprays
- Home remedies like vinegar or essential oils on irritated skin
- Scratching, even though it’s tempting
Keeping the routine simple is best.
When You Should Seek Medical Care Promptly
Try to contact a healthcare provider sooner if you notice:
- Cracks, oozing, or open sores
- Rapidly spreading redness
- Fever or chills
- Increasing pain or swelling
- No improvement after 7–10 days of antifungal treatment
These signs may indicate a bacterial infection or a condition that needs prescription medication.
How to Prevent Winter Flare-Ups in the Future
Once the rash clears, prevention becomes much easier:
- Keep the area dry daily
- Use a hair dryer on cool after showers
- Wear moisture-wicking or cotton undergarments
- Apply a light barrier before long days or exercise
- Change out of damp clothing promptly
Consistency matters more than complexity.
Conclusion
An itchy rash under the breasts during winter is uncomfortable, but it’s also very common and manageable. By focusing on gentle cleansing, thorough drying, antifungal treatment, and reducing moisture and friction, most people see noticeable improvement within a few days.
This condition is not a reflection of poor hygiene or something you’ve done wrong—it’s simply how skin folds behave under certain conditions. Taking these steps today can bring real relief while you wait to see your doctor, and they can also help prevent future flare-ups.
If symptoms persist or worsen, professional medical care is important—but for now, these practical measures can help you feel more comfortable and in control.
No Responses Yet